Definition
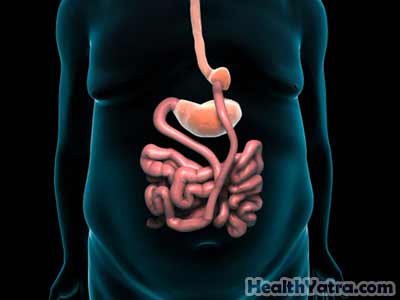
Roux-en-Y gastric bypass is a surgery for obesity. It changes the stomach and small intestine to cause weight loss by:
- Restricting food intake—creates a small pouch to serve as the stomach, so you cannot eat as much
- Making the body unable to absorb as many calories from the food—bypasses the first part of the small intestine, where many of the calories from food are usually absorbed
Reasons for Procedure
The surgery treats severe obesity. Doctors use a calculation called body mass index (BMI) to determine how overweight or obese you are. A normal BMI is 18.5-25.
Roux-en-Y gastric bypass is a weight loss option for people with:
- BMI greater than 40
- BMI 35-39.9 and a life-threatening condition, such as heart disease or diabetes
- BMI 35-39.9 with severe physical limitations that affect employment, mobility, and family life
The success of gastric bypass surgery depends on your commitment to lifelong health habits. If lifestyle changes are made and maintained, the benefits of bariatric surgery include:
- Long-term weight reduction
- Improvement in many obesity-related conditions (eg, glucose intolerance,diabetes, sleep apnea, high blood pressure, and high cholesterol)
- Improved mobility and stamina
- Enhanced mood, self-esteem, and quality of life
- Reduced risk of dying from cardiovascular disease (eg, heart attack, stroke) and other causes
Possible Complications
If you are planning to have Roux-en-Y gastric bypass, your doctor will review a list of possible complications, which may include:
- Nutritional deficiencies—You will need to take vitamins to get adequate amounts ofvitamin B12, iron, and calcium.
- Bleeding
- Infection
- Blood clots
- Hernia formation
- Bowel obstruction
- Breakdown of the staples, allowing leakage of stomach juices into the abdomen
- Diarrhea, abdominal cramping, and vomiting
- Dumping syndrome—This occurs after eating sweets, when food moves too quickly through the small intestine causing sweating, fatigue, lightheadedness, cramping, and diarrhea.
- Complications of general anesthesia
- Death—This occurs in less than 1% of patients.
Factors that may increase the risk of complications include:
- Smoking
- Recent or chronic illness (eg, kidney disease)
- Diabetes
- Old age
- Heart or lung disease
- Bleeding or clotting disorders
What to Expect
Prior to Procedure
Each bariatric surgery program has specific requirements. Your program will likely include the following:
- Thorough physical exam and review of medical history
- Attempts to lose weight (about 10%) through medically approved dietary means
- Ongoing consultations with a registered dietitian
- Mental health evaluation and counseling
Leading up to your procedure:
- Talk to your doctor about your medicines, herbs, and dietary supplements. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as warfarin (Coumadin)
- Clopidogrel (Plavix)
- Do not start taking any new medicines, herbs, or supplements without talking to your doctor.
- Arrange for a ride to and from the hospital.
- Arrange for help at home as you recover.
- You might take antibiotics before coming to the hospital.
- You might take laxatives and/or an enema to clear your intestines.
- The night before your surgery, eat a light meal. Do not eat or drink anything after midnight unless told otherwise by your doctor.
- Shower or bathe the morning of your surgery.
Anesthesia
General anesthesia will be used. You will be asleep.
Description of Procedure
To prepare you for surgery, a nurse will place an IV line in your arm. You may receive fluids and medicines through this line during the procedure. The doctor will place a breathing tube through your mouth and into your throat. This will help you breathe during surgery. You will also have a catheter placed in your bladder to drain urine.
Your doctor will make several small cuts in the abdomen. Gas will be pumped in to inflate your abdomen. This will make it easier for the doctor to see. A laparoscopeand surgical tools will be inserted through the incisions. A laparoscope is a thin, lighted tool with a tiny camera. It sends images of your abdominal cavity to a monitor in the operating room. Your doctor will operate while viewing the area on this monitor.
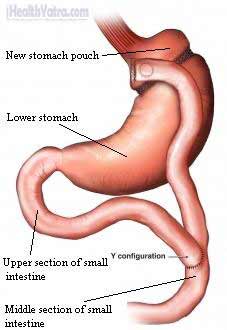
Your doctor will use surgical staples to create a small pouch at the top of your stomach. This pouch, which can hold about one cup of food, will be your new, smaller stomach. A normal stomach can hold 4-6 cups of food.
Next, the doctor will cut the small intestine and attach it to the new pouch. With the intestinal bypass, food will now move from the new stomach pouch to the middle section of the small intestine. It will skip the lower stomach and the upper section of the small intestine.
Finally, the upper section of the small intestine will be attached to the middle section of the small intestine. This will allow fluid that the lower stomach makes to move down the upper section of the small intestine and into the middle section.
Once the bypass is completed, the incisions will be closed with staples or stitches.
Be aware that in some cases, the doctor may need to switch to an open surgery. During an open surgery, she will make a larger cut in the abdomen to do the surgery.
After Procedure
You will be taken to the recovery area for monitoring. You will also be given pain medicine.
How Long Will It Take?
About two hours
How Much Will It Hurt?
Anesthesia prevents pain during surgery.
Patients experience pain and/or soreness at the incision sites during recovery. Your doctor can prescribe medicine to relieve the pain.
Average Hospital Stay
The usual length of stay is 2-5 days. Your doctor may choose to keep you longer, however, if complications arise.
Post-procedure Care
At the Hospital
While you are recovering at the hospital, you may receive the following care:
- Pain medicine will be given as needed.
- Your diet:
- On the day of surgery—You will not be given food or drinks.
- On the day after surgery—You will have an x-ray to check for leaks from the stomach pouch. For this test, you will drink a special liquid while x-rays are taken.
- If the upper GI x-ray is normal, you will be given 30 milliliters (mL) of liquids every 20 minutes.
- If leaks are found, you will receive nutrition through an IV until the leaks are fixed.
- On the second day after surgery—You will take 1-2 tablespoons of pureed food or 1-2 ounces of liquids every 20 minutes.
While in the hospital, you may be asked to do the following:
- Use an incentive spirometer to help you take deep breaths. This helps prevent lung problems.
- Wear elastic surgical stockings or boots to promote blood flow in your legs.
- Get up and walk in the hall daily.
At Home
Be sure to follow your doctor’s instructions . You will need to practice lifelong healthy eating and exercising habits. Keep in mind after your surgery:
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- You may be out of work for 2-6 weeks after gastric bypass surgery.
- Do not drive or lift anything heavy until your doctor tells you it is safe. This may be up two weeks or more.
- Walk as soon as possible, with a goal of exercising daily.
- You may have emotional ups and downs after this surgery.
- You will meet regularly with your healthcare team for monitoring and support.
Your new stomach is the size of a small egg. It is slow to empty, causing you to feel full quickly. Therefore, you need to eat very small amounts and eat very slowly:
- You will begin with 4-6 meals per day. A meal is two ounces of food.
- For the first 4-6 weeks after surgery, all food must be pureed.
- Once you move to solid foods, they must be chewed well.
- When making food choices, you will need to consume enough protein.
- Avoid sweets and fatty foods.
- Eating too much or too quickly can cause vomiting or intense pain under your breastbone. Most people quickly learn how much food they can eat.
You may need to take medicines, as directed by your doctor, which may include:
- Antacids
- Pain medicines
- Vitamin and mineral supplements
Call Your Doctor
After you leave the hospital, call your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the incision site
- Cough, shortness of breath, chest pain, or severe nausea or vomiting
- Worsening abdominal pain
- Blood in the stool
- Pain, burning, urgency or frequency of urination, or persistent bleeding in the urine
- Persistent nausea and/or vomiting
- Pain and/or swelling in your feet, calves, or legs; sudden shortness of breath or chest pain
- Any other worrisome symptoms
In case of an emergency, call for medical help right away.
