Definition
For this type of surgery, a doctor uses robotic arms to operate through small keyhole incisions in the abdomen.
The robotic arms are able to do surgical tasks with an increased range of motion. They also can filter out hand tremor. The special tools translate the doctor’s larger hand movements into smaller ones. This allows delicate work in small spaces.
Reasons for Procedure
Some laparoscopic surgeries that have been successful using robotic techniques include:
- Adrenalectomy —removal of adrenal gland
- Appendectomy —removal of the appendix
- Bariatric surgery —surgery of the stomach to treat obesity
- Cholecystectomy —removal of the gallbladder
- Colorectal procedures
- Hernia repair
- Nephrectomy —removal of a kidney
- Nissen fundoplication —surgical reinforcement of the valve between the esophagus and stomach
- Prostatectomy —removal of the prostate
- Hysterectomy —removal of the uterus (results in infertility)
- Myomectomy —removal of fibroids (noncancerous tumors in the walls of the uterus)
Compared to more traditional procedures, robotic-assisted laparoscopic surgery may result in:
- Less scarring
- Reduced recovery times
- Less risk of infection
- Less blood loss
- Reduced trauma to the body
- Shorter hospital stay
- Faster recovery
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have a robot-assisted laparoscopic procedure, your doctor will review a list of possible complications, which may include:
- Damage to neighboring organs or structures
- Infection
- Bleeding
- Anesthesia-related problems
- The need to switch to traditional surgical methods (eg, traditional laparoscopic or open surgery)
Some factors that may increase the risk of complications include:
Factors that may increase the risk of complications include:
- Smoking
- Pre-existing heart or lung condition
- Obesity
- Diabetes
- Excessive alcohol intake
- Previous abdominal or pelvic surgery
- Use of certain medicines
Be sure to discuss these risks with your doctor before the procedure.
What to Expect
Prior to Procedure
Depending on the reason for your surgery, your doctor may do the following:
- Physical exam
- Blood tests
- Urine tests
- Electrocardiogram (ECG, EKG) —a test that records the electrical currents passing through the heart muscle
- Intravenous pyelogram (IVP) —a type of x-ray that creates images of the kidney, ureters, and bladder by injecting dye into the bloodstream
- Kidneys, ureter, bladder (KUB) —an x-ray of the abdomen
- Abdominal or pelvic ultrasound —a test that uses sound waves to visualize the inside of the body
- CT scan —a type of x-ray that uses a computer to create images of structures inside the abdomen or pelvis
Leading up to the procedure:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Anti-inflammatory drugs (eg, aspirin )
- Blood thinners such as clopidogrel (Plavix) or warfarin (Coumadin)
- Take antibiotics if instructed.
- Take a laxative and/or use an enema to clean out your intestines if instructed.
- Follow a special diet if instructed.
- Shower the night before using antibacterial soap if instructed.
- Arrange for someone to drive you home from the hospital. Also, have someone to help you at home.
- Eat a light meal the night before. Do not eat or drink anything after midnight.
Anesthesia
Depending on the type of procedure that you have, you may be given:
- General anesthesia —blocks pain and keeps you asleep through the surgery
- Local anesthesia—just the area that is being operated on is numbed; given as an injection and may also be given with a sedative
Description of the Procedure
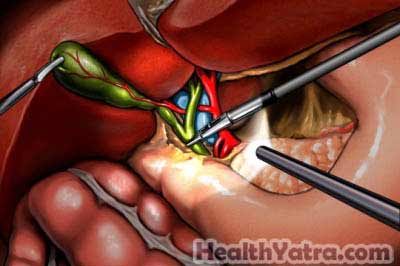
Several small incisions will be made. They are called keyhole incisions. Carbon dioxide gas will be passed into the abdomen to expand it. This will make it easier for the doctor to see.
A small camera will be passed through one of the incisions. This tool is called an endoscope. It lights, magnifies, and projects an image of the organs onto a video screen. The endoscope will be attached to one of the robotic arms. The other arms will hold tools that are able to grasp, cut, dissect, and suture. These may include:
- Forceps
- Scissors
- Dissectors
- Scalpels
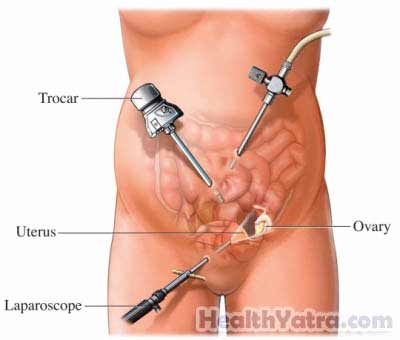
The doctor will sit at a console, looking at the images on the screen. Joystick-like hand controls and foot pedals will help to guide the tools. Another doctor will stay by you to adjust the tools as needed. In some cases, organs or tissue might need to be removed. When the procedure is done, the tools will be removed. The doctor will close the incisions with sutures or staples and apply a sterile dressing.
How Long Will It Take?
About 1-2 hours (depending on the type of procedure)
How Much Will It Hurt?
You will have pain and discomfort during recovery. Your doctor will give you pain medicine. You may also feel bloated or have pain in your shoulder from the gas used during the procedure. This can last up to three days.
Average Hospital Stay
This procedure is done in a hospital setting. The usual length of stay is 1-2 days. Your doctor may choose to keep you longer if you have any problems.
Post-procedure Care
When you return home, do the following to help ensure a smooth recovery:
- Wash the incisions with mild soap and water.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Take antibiotics to help prevent infection if instructed.
- Avoid certain medicines.
- Resume normal activities (eg, daily walks) soon. This will promote healing. You will have to avoid other activities, like driving, sexual activity, and strenuous exercise.
- Gradually progress from a liquid to a solid diet.
- To avoid constipation:
- Eat a high-fiber diet.
- Drink plenty of water.
- Use stool softeners.
- Be sure to follow your doctor’s instructions.
Depending on the procedure, you should make a full recovery within a few weeks.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from an incision site
- Abdominal swelling or pain
- Severe nausea or vomiting
- Persistent diarrhea or constipation
- Blood in the stool
- Pain and/or swelling in your feet, calves, or legs
- Cough, shortness of breath, chest pain
- Difficulty urinating, such as pain, burning, urgency, frequency, or persistent bleeding
- Being unable to eat or drink liquids
- Headache, feeling faint or dizzy
- Excessive vaginal bleeding (soaking more than one pad per hour) after a gynecologic procedure
- Persistent or foul smelling vaginal discharge after a gynecologic procedure
- Other worrisome symptoms
In case of an emergency, call for medical help right away.
