Definition
A doctor guides robotic arms to do surgery on the heart. The surgery is done through several tiny keyhole incisions.
Reasons for Procedure
Robot-assisted cardiac procedures are done to treat a variety of conditions:
- Robot-assisted mitral valve repair may be used to treat:
- Stenosis (narrowing) of the mitral valve
- Regurgitation (leakage) of the mitral valve
- Robot-assisted coronary artery bypass grafting (CABG) may be used to treat:
- Blockages in the heart’s arteries
- Severe chest pain ( angina) that has not improved with medicines
- Robot-assisted atrial septal defect repair may be used to treat a hole between the upper chambers of the heart that does not close properly during fetal development.
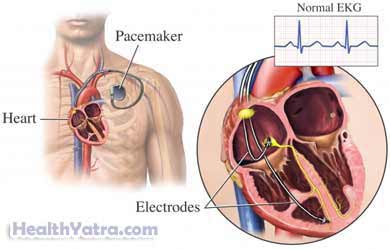
- Robot-assisted biventricular pacemaker lead placement may be used to treat heart failure due to atrial fibrillation (irregular heart rhythm in the upper chambers of the heart).
Benefits of robot-assisted cardiac procedures may include:
- Increased range of motion with the robotic arms
- Ability to filter out human hand tremor and translate the doctor’s larger hand movements into smaller ones
- Reduced trauma to the body
- Shorter hospital stay
- Faster recovery
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have a robot-assisted cardiac procedure, your doctor will review a list of possible complications, which may include:
- Damage to neighboring organs or structures in the chest
- Infection
- Bleeding
- Blood clots
- Anesthesia-related problems
- Death
Some factors that may increase the risk of complications include:
- Prior heart attack or heart surgery
- Advanced age
- Diabetes
- Obesity
- Smoking
- Excessive alcohol intake
- Uncontrolled thyroid disease
Be sure to discuss these risks with your doctor before the surgery.
What to Expect
Prior to Procedure
Depending on the reason for your surgery, your doctor may do the following:
- Physical exam
- Blood and urine tests
- Electrocardiogram (ECG, EKG) —a test that records the electrical currents passing through the heart muscle
- Coronary angiogram —a test to determine the extent and location of blockages of blood vessels supplying the heart muscle
- Chest x-ray —a test that uses radiation to take a picture of structures inside the chest
- Ultrasound —a test that uses sound waves to visualize structures inside the chest
- CT scan —a type of x-ray that uses a computer to create images of structures inside the chest
- MRI scan —a test that uses magnetic waves to make pictures of structures inside the chest
Leading up to the procedure:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, such as:
- Anti-inflammatory drugs (eg, aspirin )
- Blood thinners, like clopidogrel (Plavix) or warfarin (Coumadin)
- Take antibiotics if instructed.
- Follow a special diet if instructed.
- Shower the night before using antibacterial soap if instructed.
- Arrange for someone to drive you home from the hospital. Also, have someone to help you at home.
- Eat a light meal the night before. Do not eat or drink anything after midnight.
Anesthesia
There are two options for anesthesia:
- General anesthesia —blocks pain and keeps you asleep through the surgery
- Local anesthesia with sedation—just the area that is being operated on is numbed, given as an injection
Description of the Procedure
The doctor will cut several keyhole openings in the spaces between the ribs. Next, the doctor will pass a small camera through one of the incisions. This small camera is called an endoscope. It will light, magnify, and project an image of the organs onto a monitor. The endoscope will be attached to one of the robotic arms. The other arms will hold instruments for grasping, cutting, dissecting, and suturing. These may include:
- Forceps
- Scissors
- Dissectors
- Scalpels
While sitting at a console near the operating table, the doctor will look through lenses. He will see magnified 3D images of the inside of the chest. Another doctor will stay by the operating table and adjust the camera and instruments. The console will have joystick hand controls and foot pedals. Using these, the doctor will guide the robotic arms and instruments. After the instruments are removed, incisions will be closed with sutures or staples.
Immediately After Procedure
After the procedure, you will be:
- Moved to the intensive care unit (ICU)
- Closely monitored
- Encouraged to sit up and move around soon after surgery
How Long Will It Take?
Usually 1-4 hours (depending on the procedure)
How Much Will It Hurt?
You will have pain and soreness during recovery. Ask your doctor about pain medicine.
Average Hospital Stay
This procedure is done in a hospital setting. The usual length of stay is dependent on the procedure you had done. Your doctor may need to keep you longer if you have any problems.
Post-procedure Care
When you return home, do the following to help ensure a smooth recovery:
- Follow your doctor’s guidelines on taking medicine. You may need to take antibiotics.
- Do deep breathing and coughing exercises.
- Follow a special diet.
- Wash the incisions with mild soap and water.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Limit certain activities (eg, driving, strenuous activity).
- Enroll in a cardiac rehabilitation program.
- Be sure to follow your doctor’s instructions.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from an incision site
- Cough, shortness of breath, or chest pain
- Difficulty urinating, such as pain, burning, urgency, frequency, or bleeding
- Severe nausea or vomiting
- Rapid weight gain
- Pain and/or swelling in your feet, calves, or legs
- Headache, feeling faint or dizzy
- Other worrisome symptoms
In case of an emergency, call for medical help right away.
