Definition
Dialysis is a treatment that takes over the job of your kidneys if they fail. The kidneys have many functions that help your body stay healthy. They help clear toxins out of your blood and help your body balance salt levels. Most patients begin dialysis when their kidneys have lost 85%-90% of their ability. You may be on dialysis for a short time, or you may need it for the rest of your life (or until you receive a kidney transplant), depending on the reason for your kidney failure.
If you have kidneys that are not working and the damage is not reversible, you haveend-stage renal disease (ESRD). ESRD is caused by conditions such as diabetes,kidney cancer, drug use, high blood pressure, or other kidney problems. Dialysis is not a cure for ESRD, but it does help you feel better and live longer.
There are two types of dialysis: hemodialysis and peritoneal dialysis. This fact sheet will focus on peritoneal dialysis.
Reasons for Procedure
The main functions of peritoneal dialysis are to:
- Remove waste and excess fluid from your blood
- Control blood pressure
- Keep a safe level of salts in the body, such as potassium, sodium, and chloride
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have peritoneal dialysis, your doctor will review a list of possible complications. These may include:
- Lowering your red blood count and causing anemia
- Muscle cramps
- Nausea, vomiting
- Headaches
- Feeling hot, sweaty, weak, and/or dizzy
- Infection of the abdominal cavity
- Inflammation of the heart sac ( pericarditis)
- Neurologic problems
- Disruption of calcium and phosphorus balance, resulting in weakened bones
Factors that may increase the risk of complications include:
- Adhesions or significant abdominal scar tissue
- Infection of the peritoneum (lining of the abdominal cavity)
- Abdominal hernia
- Diverticulitis —an infection of a pouch that forms in the wall of the large intestine
- Abdominal defects
What to Expect
Prior to Procedure
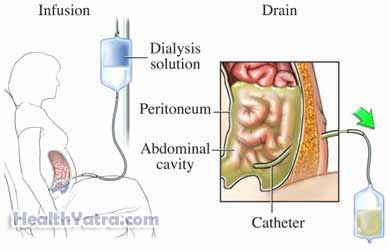
Before the first treatment, a small, soft tube (approximately 24 inches long) will be placed in the abdomen. This tube will remain there permanently. A portion of the tube remains outside the body for use in the process. It is important to keep this access clean and dry to prevent infection.
Description of the Procedure
Peritoneal dialysis can often be done at home.
The abdominal lining is called the peritoneal membrane. It is used to filter blood. A cleansing solution, called a dialysate, is inserted into your abdominal cavity through a tube. Fluid, wastes, and chemicals pass from the tiny blood vessels in the peritoneal membrane into the dialysate. The dialysate is drained after several hours. New dialysate can be added to repeat the process.
There are three types of peritoneal dialysis:
- Continuous ambulatory peritoneal dialysis (CAPD) —This is the most common type of peritoneal dialysis. A bag of dialysate is infused into the abdomen through a tube called a catheter. It remains there for 3-6 hours and is drained. The abdomen is refilled with fresh solution. This way, your blood is always being cleaned.
- Continuous cyclical peritoneal dialysis (CCPD) —Infusing and refilling the abdomen with dialysate is done by machine. It is done at night while you are sleeping.
- Intermittent peritoneal dialysis (IPD) —This uses the same type of machine as CCPD. It requires assistance and is usually done at a hospital or center. It often takes longer than CCPD.
How Long Will It Take?
The time needed for peritoneal dialysis depends on a few factors:
- How much kidney function remains
- How much fluid weight gain has occurred since the last treatment
- Amount of waste in the body
- Body size
- Level of salts in your body, such as sodium, potassium, and chloride
- Peritoneal dialysis type used
The approximate time and frequency of each type:
| Type | Length of Procedure | Frequency of Procedure |
|---|---|---|
| CAPD | 3-6 hours, plus 30 minutes to drain | 4 times/day |
| CCPD | 9-12 hours | Every night |
| IPD | 12 + hours | 36-42 hours/week |
Will It Hurt?
In general, peritoneal dialysis does not cause pain.
Post-procedure Care
At Home
Be sure to follow your doctor’s instructions . There are some special considerations:
Dietary Guidelines
Certain dietary guidelines should be followed. This will help to maintain overall health and optimize treatment effects. Talk to your doctor about your specific dietary needs.
Medications
Your doctor may give you various medicines. These include, but are not limited to:
- Blood pressure medicines
- Calcium supplements or multivitamins
- Phosphorus binders—to lower phosphorus levels in the blood
- Diuretics—to remove excess fluid
- Stool softeners or laxatives—to prevent or treat constipation, which can be caused by decreased fluid intake
- Iron supplements—to increase iron intake, which is important for production of red blood cells
- Medicines to stimulate the body to produce more red blood cells
Call Your Doctor
Contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, warmth, increasing pain, excessive bleeding, or discharge at the catheter or tube insertion site
- Blood or cloudiness in the peritoneal dialysis fluid
- Nausea or vomiting
- Abdominal pain
- Dizziness or weakness
In case of an emergency, call for medical help right away.
