Definition
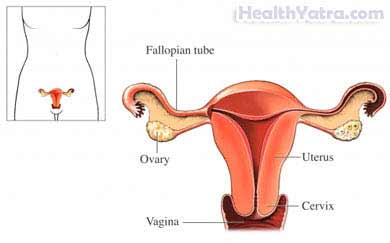
This procedure uses a hysteroscope to view the inside of a woman’s uterus (womb). A hysteroscope is a long, thin telescope with a camera on the end. Other small, surgical tools may also be inserted into the uterus through the hysteroscope.
Reasons for Procedure
Hysteroscopy is done for:
- Diagnostic reasons—to examine the inner uterus to identify problems or abnormalities; may be done if you have:
- Repeated miscarriages
- Infertility
- An abnormal Pap test
- Abnormal or postmenopausal uterine bleeding
- Therapeutic reasons—to correct anatomic problems and defects in the uterus; may be done for:
- Endometrial ablation —removal of uterine lining from the uterus
- Myomectomy —removal of fibrous or muscular tissue (fibroids)
- Removal of polyps (usually noncancerous)
- Removal of intrauterine devices (IUDs)
The result of the hysteroscopy depends on the reason for the procedure. In some cases, the doctor may be able to treat a condition right away. In other cases, you may need further surgery or other treatment.
Possible Complications
Complications are rare. But, no procedure is completely free of risk. If you are planning to have hysteroscopy, your doctor will review a list of possible complications. These may include:
- Swelling or bleeding
- Infection
- Organ injury
- Reaction to anesthesia
Factors that may increase the risk of complications include:
- History of pelvic inflammatory disease
- Inflammation of the cervix
- Distended bladder
- Pregnancy or possible pregnancy
- Allergies to surgical materials (eg, iodine, latex, medicines, anesthetics)
Be sure to discuss these risks with your doctor before the procedure.
What to Expect
Prior to Procedure
Your doctor will ask about your medical history, medicines, and allergies. A physical exam will be done. Blood tests may also be done.
Leading up to the procedure:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Anti-inflammatory drugs (eg, aspirin)
- Blood thinners, such as clopidogrel or warfarin
- Arrange to have someone drive you home. Also, arrange for help at home.
- If instructed, eat a light meal the night before the surgery. Do not eat or drink anything after midnight.
Anesthesia
Depending on the reason for the hysterscopy, your doctor may use:
- General anesthesia —blocks pain and keeps you asleep through the surgery; used for therapeutic procedure
- Regional anesthesia—numbs one area of the body; used for diagnostic or therapeutic procedure
- Local anesthesia—just the area that is being operated on is numbed; given as an injection and may also be given with a sedative; used for diagnostic procedure
Description of the Procedure
A device called a speculum will be inserted into the vagina. It will hold your vagina open and allow instruments to enter easily. The doctor will clean the vagina and may dilate the cervix. The hysteroscope will then be put into the uterus through the vagina and dilated cervix. The uterus will be filled with carbon dioxide gas or a liquid. This will cause the uterus to inflate, allowing the doctor to get a closer, clear look at the uterine walls.
If you are having the procedure done for diagnostic reasons, the doctor will examine the uterus for abnormal tissue. A biopsy may be taken. Or, the uterine walls may be swabbed to get cell samples.
If you are having the procedure done for therapeutic reasons, the doctor may insert small surgical tools through the hysteroscope. The doctor will use the tools to remove diseased tissue and make repairs. In some cases, the doctor will use another viewing tube called a laparoscope. It will be passed into the abdomen. This allows the doctor to monitor the outside of the uterus and detect any possible perforation of the uterus by the hysteroscope.
How Long Will It Take?
About 15-45 minutes (or longer for therapeutic procedure)
How Much Will It Hurt?
You will have mild cramping and soreness. Ask your doctor about pain medicine.
Post-procedure Care
When you return home after the procedure, do the following to help ensure a smooth recovery:
- Rest as needed. Ask for someone to help you at home.
- Recovery time is short. Return to your normal activities the day after the procedure.
- Do not take medicine without your doctor’s approval. Some medicines may make bleeding worse.
- You may have difficulty using the bathroom for a few hours after the procedure. You may also have watery or bloody vaginal discharge for 3-4 weeks.
- You may have some bleeding or discharge from your vagina for several days postsurgery. A sanitary napkin or pad may be worn.
- Talk to your doctor about when it is okay to have sex, use tampons, or put anything else in the vagina.
- Be sure to follow your doctor’s instructions .
Call Your Doctor
After arriving home, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Abnormal bleeding (more than a menstrual period)
- Foul-smelling vaginal discharge
- Abdominal pain
- Nausea, vomiting
- Cough, shortness of breath, difficulty swallowing, or chest pain
- Trouble urinating
- Any other concerns
In case of an emergency, call for medical help right away.
