Definition
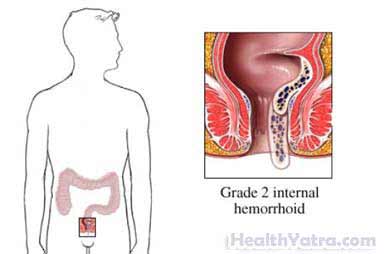
Hemorrhoids are enlarged, bulging blood vessels in the anus and lower rectum. Hemorrhoid banding is a procedure to remove them.
Reasons for Procedure
Banding is used to treat painful, swollen hemorrhoids. The procedure is most often done for the following reasons:
- Severely bleeding hemorrhoids
- Severely painful hemorrhoids
- Hemorrhoid containing a blood clot (thrombosed hemorrhoid)
- Hemorrhoids that protrude through the anus (prolapsed hemorrhoids)
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have hemorrhoid banding, your doctor will review a list of possible complications, which may include:
- Infection
- Bleeding
- Recurrence of hemorrhoids
- Swelling and pain from remaining hemorrhoids
- Adverse reaction to the local anesthetic (if used)
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Rectal exam
- Anoscopy—the visual examination of the inside of the anus using a short tube (anoscope) to help keep the sphincter open
- Sigmoidoscopy—the use of a specialized endoscope (a tube attached to a viewing device) to examine the inside of the anus, rectum, and lower intestine
Anesthesia
The procedure does not typically call for anesthesia. A local anesthesia may be used in some cases to numb the area.
Description of the Procedure
An anoscope will be inserted through the anus. The doctor will look through the tube to see inside the rectum and locate the hemorrhoid. The doctor will then use a special banding tool. The tool will place a small rubber band around the hemorrhoid. The band cuts off the blood supply. This will make the hemorrhoid fall off. More than one hemorrhoid may be banded. The band and the hemorrhoid will fall off in about 1-2 weeks.
How Long Will It Take?
This is a relatively quick procedure. The length of time depends on how many hemorrhoids need treatment.
Will It Hurt?
Patients often report some discomfort during and after this procedure. If you feel sharp or severe pain, tell the doctor immediately. Mild pain medicine will help you manage discomfort during recovery.
Post-procedure Care
For a few days, you may have difficulty controlling the passage of gas and bowel movements. When you return home after the procedure, do the following to help ensure a smooth recovery:
- Ask your doctor about when it is safe to shower, bathe, or soak in water. If your doctor says it is okay, take sitz baths as recommended. Sitz baths will help relieve discomfort and clean the area. For a sitz bath, sit in warm water for 10-15 minutes. Pat the area dry. Do not wipe or rub vigorously. You may be advised to take a sitz bath every four hours and after every bowel movement. Devices are available to place on top of the toilet to make this process easier.
- Move your bowels as soon as you feel the urge.
- Do not strain, bear down, or hold your breath during a bowel movement.
- Do not sit on the toilet for long periods of time.
- To prevent constipation and straining during bowel movements, use a stool softener, exercise, drink plenty of fluids, and eat plenty of high-fiber foods (such as fruits, vegetables, beans, and whole grains).
- Apply creams or ointments as directed by your doctor.
- Avoid heavy lifting for two or three weeks.
- Be sure to follow your doctor’s instructions.
Expect some bleeding when the hemorrhoid falls off. See your doctor for a follow-up 3-4 weeks after the procedure.
Call Your Doctor
After arriving home, contact your doctor if any of the following occurs:
- Passing large amounts of blood
- Signs of infection, including fever and chills
- Pain that you cannot control with the medicines you have been given
- Constipation or trouble urinating
- An aching feeling develops in the area between the rectum and the genitals
In case of an emergency, call for medical help right away.
