Definition
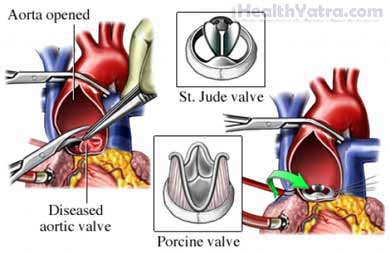
This is surgery to replace a damaged heart valve. The heart’s four valves open and tightly close. The tricuspid and mitral valves allow blood to flow from one chamber to another. The pulmonary and aortic valves allow blood to flow to the large blood vessels. The valves make it so that blood can only flow forward when the heart squeezes. Usually, only one valve is replaced at a time. But, at times, one or more valves may need to be replaced. The new heart valves can be:
- Mechanical, made of metal and plastic, such as a St. Jude valve
- Made of tissue—most commonly from a pig or a cow, but they may also be supplied by a human donor or even made from your own tissue
Reasons for Procedure
This procedure is done to repair a valve that is not functioning properly due to:
- Congenital defects
- Narrowed, stiff valves that obstruct the free flow of blood
- Loose, leaky valves that allow blood to flow the wrong way through the heart
- Infected heart valves
Possible Complications
If you are planning to have heart valve replacement, your doctor will review a list of possible complications, which may include:
- Infection
- Blood clots forming around the valve, which can cause a stroke,, myocardial infarction, kidney damage, or damage to the extremities
- New valve does not work properly
- Bleeding
- Anesthesia-related problems
- Death
Some factors that may increase the risk of complications include:
- Smoking
- Pre-existing heart or lung condition
- Increased age
- Recent or long-term illness
- Recent infection
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Echocardiogram —a test that uses sound waves to visualize functioning of the heart, including the valves
- X-ray —a test that uses radiation to take a picture of structures inside the body
- Electrocardiogram (ECG, EKG)—a test that records the heart’s activity by measuring electrical currents through the heart muscle
- Cardiac catheterization —the insertion of a tube-like instrument into the heart through an artery to detect problems with the heart and its blood supply. It can also accurately define the valve problem.
Leading up to your procedure:
- If you had to stop medicines before the procedure, ask your doctor when you can start again. Medicines often stopped include:
- Anti-inflammatory drugs
- Blood thinners
- Arrange for a ride to and from the hospital.
- Arrange for help at home after the surgery.
- Eat a light meal the night before the surgery. Do not eat or drink anything after midnight.
Anesthesia
General anesthesia will be used. It will block any pain and keep you asleep through the surgery. It is given through an IV.
Description of the Procedure
The doctor will cut through the skin and breastbone. The chest cavity will be opened. Next, your heart will be connected to a heart-lung machine. This machine will take over the functions of the heart and lungs during the surgery. Next, the heart will be stopped. An incision will be made and the damaged valve will be removed. The new valve will be stitched into place. The doctor will check to make sure the valve opens and closes properly. The incision in the heart will be closed, and the heart will be restarted. After the heart is working fine, you will be removed from the heart-lung machine. The chest will be closed with wires. Lastly, the skin will be closed with sutures.
Immediately After Procedure
You will be closely monitored in the intensive care unit (ICU) with the help of the following devices:
- A heart monitor
- A breathing tube—until you can breathe on your own
- Chest tubes—to drain accumulated fluids from the chest
- A line into an artery in your arm or leg—to measure pressure
- A tube through your nose and into the stomach—to keep the stomach drained of accumulated fluids and gas
- An IV to deliver fluids and medications
- A bladder catheter
How Long Will It Take?
3-5 hours—depending on how many valves need to be replaced
How Much Will It Hurt?
You will have pain while recovering. Your doctor will give you pain medicine.
Average Hospital Stay
This procedure is done in a hospital setting. The usual length of stay is 2-5 days. The first day is spent in ICU. Your doctor may choose to keep you longer if complications occur.
Post-procedure Care
At the Hospital
While you are recovering at the hospital, you may be instructed to:
- Breathe deeply and cough 10-20 times every hour to help keep your lungs working well.
- Walk with assistance. You may be encouraged to walk 2-3 days after surgery.
- Take blood thinners to prevent blood clots from forming around the valve. If you have a tissue valve, you will not need a blood thinner. If you have a mechanical valve, you will have to take the medicine for the rest of your life.
At Home
When you return home, do the following to help ensure a smooth recovery:
- Gradually resume your regular diet.
- Work with a physical therapist.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions .
The surgical site in your breastbone will heal in 4-6 weeks. After the recovery process, you should be able to return to normal activities.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the incision site
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Pain that you cannot control with the medicines you have been given
- Cough, shortness of breath, or chest pain
- Coughing up blood
- Rapid heart rate
- Sudden headache or feeling faint
- Problems with vision or speaking
- Numbness or weakness on one side of your body
- Inability to urinate
- Pain, burning, urgency, frequency of urination, or persistent bleeding in the urine
- Pain and/or swelling in your feet, calves, or legs
In case of an emergency, call for medical help right away.
