Definition
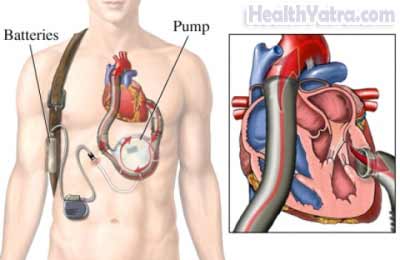
A heart assist system implantation (also called a ventricular assist device, or VAD) is an artificial heart. This single-chamber artificial heart works by compressed air or battery power. The device boosts the function of a failing heart ventricle.
Reasons for Procedure
Heart failure occurs when the heart is too weak to pump all the blood it receives and blood begins to back up. Blood can back up into the lungs and into the lower parts of the body. This can trouble breathing, cough, and swelling of the legs and ankles.
Getting a VAD is a way to improve the heart’s ability to pump without having a heart transplant. A VAD is sometimes referred to as a bridge to transplant, since it can be used to maintain people awaiting a heart transplant. This device can also be used for permanent treatment in people who:
- Are not candidates for transplant
- Do not respond to standard treatment
- Have a low risk of surviving one year
Possible Complications
If you are planning to have VAD implantation, your doctor will review a list of possible complications, which may include:
- Bleeding
- Blood clots
- Infection
- Device failure
- Adverse reaction to the anesthesia
- Kidney, lung, or heart damage
Factors that may increase the risk of complications include having:
- A serious infectious disease
- Advanced disease of vital organs other than the heart
- Blood clotting disorder
Also, if you have a small stature, you may not be able to get a VAD. The device is bulky. Newer generation continuous flow devices, which are much smaller, are being studied.
Be sure to discuss these risks with your doctor before the surgery.
What to Expect
Prior to Procedure
If you need a VAD, it is because your heart is failing. Most likely, you will be on a list to receive a heart transplant. You may already be in the hospital. Your doctor will do many tests, for example:
- Echocardiogram —size, shape, and motion of the heart are examined using sound waves
- X-ray —uses radiation to take a picture of structures inside the body
- Cardiac Catheterization —to look for coronary artery disease
- Psychological and social system evaluations to make sure you are prepared to manage the device outside of the hospital
Leading up to the procedure, your doctor will instruct you to:
- Avoid eating for 8 hours before the procedure
- Stop taking aspirin or other anti-inflammatory drugs for one week before surgery. You may also need to stop taking blood-thinning medicines, such as:
- Clopidogrel (Plavix)
- Warfarin (Coumadin)
Anesthesia
General anesthesia will be used. It will block any pain and keep you asleep through the surgery.
Description of the Procedure
This procedure involves open heart surgery. The doctor will make an incision down the length of your breast bone. The breast bone will then be split and separated. You will be placed on a heart-lung machine. This machine will take the place of your heart and lungs during the surgery. The doctor will place the VAD into a pocket on the inside of the abdominal wall. The device will be sewn into your heart. It may also be sewn into your aorta, depending on the type of device.
Immediately After Procedure
You will be in the intensive care unit (ICU) after the procedure. You will be connected to many tubes. The medical staff will monitor you.
How Long Will It Take?
About 4-8 hours
How Much Will It Hurt?
You will have pain from the surgery. Ask your doctor about medicine to help with the pain.
Average Hospital Stay
- 2-5 days in the ICU
- 2-4 weeks in a regular hospital room
Postoperative Care
At Home
When you return home, do the following to help ensure a smooth recovery:
- Stay in contact with the heart center. You may be waiting for a heart transplant.
- Slowly increase your activity as instructed. Ask your doctor if you will be able to return to work.
- As prescribed by your doctor, take blood thinners. These will prevent blood clots.
- Be sure to follow your doctor’s instructions. She will tell you:
- How to take care of your VAD
- When to contact the hospital—Make sure that you know how to call your doctor if you have an emergency.
Ask your doctor about when it is safe to shower, bathe, or soak in water.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision site
- Increasing pain
- One-sided weakness, blurry vision, or inability to talk
- A cold, pale or blue, numb, or painful extremity
- Cough, difficulty breathing, or chest pain
- Nausea, vomiting
- Problems with urination or bowel movements
- Redness or swelling in legs.
- Warning indications from the device
In case of an emergency, call for medical help right away.
