Definition
Fundoplication is a surgery on the stomach and esophagus. It is done to treatgastroesophageal reflux disease (GERD). GERD is also called acid reflux or heartburn. This occurs when acid from the stomach goes up the esophagus. A hiatal hernia may also be fixed during the procedure. This type of hernia occurs when a portion of the stomach pokes into the chest cavity. This hernia increases the chance and severity of GERD.
Reasons for Procedure
The surgery is most often done for the following reasons:
- Eliminate persistent GERD symptoms that are not relieved by medicine
- Correct acid reflux that is contributing to asthma symptoms
- Repair a hiatal hernia, which may be responsible for making GERD symptoms worse
- Eliminate the source of serious, long-term complications resulting from too much acid in the esophagus
Possible Complications
If you are planning to have fundoplication, your doctor will review a list of possible complications, which may include:
- Infection
- Bleeding
- Difficulty swallowing
- Return of reflux symptoms
- Limited ability to burp or vomit
- Gas pains
- Damage to organs
- Anesthesia-related problems
In rare cases, the procedure may need to be repeated. This may happen if the wrap was too tight, the wrap slips, or if a new hernia forms.
Some factors that may increase the risk of complications include:
- Pre-existing heart or lung condition
- Obesity
- Smoking
- Diabetes
- Prior upper abdominal surgery
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- X-ray —a test that uses radiation to take a picture of structures inside the body, especially bones
- Endoscopy —use of a tube attached to a viewing device (an endoscope) to examine the inside of the lining of the esophagus and stomach; a biopsy may also be taken
- Manometry—a test to measure the muscular contractions inside the esophagus and its response to swallowing
Leading up to the surgery:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Anti-inflammatory drugs (eg, aspirin )
- Blood thinners, like warfarin (Coumadin)
- Clopidogrel (Plavix)
- Arrange for a ride to and from the hospital. Also, arrange for help at home.
- The night before, eat a light meal. Do not eat or drink anything after midnight.
Anesthesia
General anesthesia will be used. It will block any pain and keep you asleep through the surgery.
Description of the Procedure
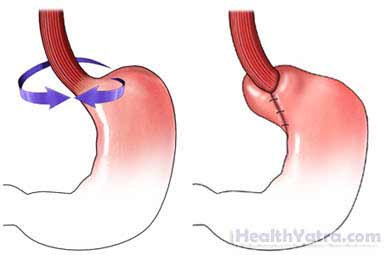
Open Procedure/Nissen Fundoplication
A wide incision will be made in the abdomen. This is to expose the stomach and lower esophagus. The doctor will wrap the upper portion of the stomach around the esophagus. This will create pressure on the lower part of the esophagus. It will prevent stomach acid from moving up the esophagus. If a hiatal hernia exists, the stomach will be placed entirely back in the abdomen. The doctor will then tighten the opening in the diaphragm where the hernia poked through.
How Long Will It Take?
2-4 hours
How Much Will It Hurt?
You will have discomfort during recovery. Ask your doctor about medicine to help with the pain.
Average Hospital Stay
2-4 days
Post-procedure Care
- Walk with assistance the day after surgery.
- Keep the incision area clean and dry.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- You will start by eating a liquid diet. You will slowly be able to eat more solid foods.
- After a successful fundoplication, you may no longer need to take medicines for GERD.
- Be sure to follow your doctor’s instructions .
It will take about six weeks to recover.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision site
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Increased swelling or pain in the abdomen
- Difficulty swallowing that does not improve
- Pain that you cannot control with the medicines you have been given
- Pain, burning, urgency or frequency of urination, or persistent bleeding in the urine
- Cough, shortness of breath, or chest pain
- Any other new symptoms
In case of an emergency, call for medical help right away.
