Definition
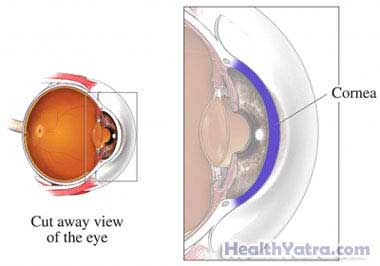
This is a surgical procedure used to replace a portion of a diseased or damaged cornea with a healthy one. The cornea is the clear, outer surface on the front of the eye. The surgery is done by an ophthalmologist, a doctor who specializes in treating eye problems.
Reasons for Procedure
A corneal transplant can correct vision problems caused by infections, injuries, or medical conditions. It is often recommended for the following:
- Keratoconus—a thinning of the cornea that causes blurred vision
- A cornea scarred from infection or injury
- Clouding of the cornea
Most people who undergo a corneal transplant enjoy improved vision for many years, or even a lifetime. It can take up to a year for vision to stabilize after surgery. Most people still need to wear glasses or contacts.
Possible Complications
The procedure is highly successful. Severe complications are rare. If you are planning to have a corneal transplant, your doctor will review a list of possible complications, which may include:
- Rejection of the new cornea—The body’s defense system attacks the new tissue, damaging it.
- Glaucoma —This is a vision-impairing disease caused by increased pressure inside the eye.
- Problems focusing
- Swelling or detachment of the retina —The retina is the part of the eye that sends light and images to the brain via the optic nerve (detachment occurs when the retina is lifted or pulled from its normal position).
- Cataract —A clouding of the eye’s lens leads to decreased vision.
- Infection
- Bleeding
The operation is most successful for patients who have the following:
- Keratoconus
- Corneal scars
It is less successful for those who have corneal infection and severe injury, like a chemical burn.
What to Expect
Prior to Procedure
Your ophthalmologist may do the following:
- Physical exam
- Blood tests
Before the procedure:
- Talk to your doctor about your medicines. Also, discuss any herbs or vitamins you take. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as clopidogrel (Plavix) or warfarin (Coumadin)
- Arrange to have someone drive you home.
- Arrange for help at home after the procedure.
- Use any eye drops as instructed by your ophthalmologist.
- The day before, do not eat or drink anything after midnight (unless told otherwise by your doctor).
Anesthesia
Two types of anesthesia can be used during a corneal transplant:
- Local anesthesia (most commonly used) to numb the eye—You will stay awake.
- General anesthesia —You will be asleep.
Description of Procedure
The procedure will be done under a surgical microscope. The damaged part of the cornea will be cut out. The new cornea will then be placed in the opening. The new cornea will be fastened with very fine stitches. Finally, a patch and shield will be put over the eye.
There is a newer technique, called Descemet’s stripping endothelial keratoplasty (DSEK). DSEK is used for some types of cornea transplants. It may result in shorter recovery time and better vision. With this technique, the doctor removes a much smaller part of the cornea, compared with older procedures. DSEK is not widely available yet in the US, but it is becoming more popular.
How Long Will It Take?
1-2 hours
How Much Will It Hurt?
Anesthesia prevents pain during surgery. You may have slight soreness for a few days after the procedure. Ask your doctor about medicine to help with the pain.
Average Hospital Stay
You will most likely go home after a few hours in the recovery area.
Post-procedure Care
At Home
After you leave the hospital, you should rest for the remainder of the day. When you return home after the procedure, do the following to help ensure a smooth recovery:
- Continue to wear the eye patch until your doctor instructs you to remove it.
- Use eye drops as prescribed.
- Wear glasses during the day, and wear a shield to protect your eye at night.
- Protect your eye from accidental bumps or pokes.
- Do not rub or press on your eye.
- Do not swim until allowed by your doctor.
- Avoid contact sports.
- Do not drive until your doctor gives you permission.
- Be sure to follow your doctor’s instructions .
Your eye will be checked several times during the following weeks and months. Stitches are usually left in place for at least several months.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Vision symptoms, including decreased vision, floaters, flashing lights, increased light sensitivity, or loss of peripheral vision
- Increased eye redness
- Increased pain
- Cough, shortness of breath, or chest pain
- Nausea or vomiting
In case of an emergency, call for medical help right away.
