Definition
Breast augmentation is a surgery to increase the size or change the shape of your breasts.
Reasons for Procedure
- Cosmetic reasons—to increase breast size, make breasts symmetric, or improve breast shape and/or contour
- Reconstructive reasons—to increase the size of breasts that have been injured or after surgery (eg, following mastectomy for breast cancer)
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have a breast augmentation, your doctor will review a list of possible complications, which may include:
- Bleeding
- Infection
- Pain
- Abnormal scarring
- Painful and/or restricted arm and shoulder motion
- Uneven appearance of breasts, either due to position or size
- Implant hardens, ruptures, leaks, or deflates
- Implant may make cancer detection (through mammogram and/or self-exam) more difficult
- Decreased sensation
- The need to have more surgeries, including having the implants removed
Factors that may increase the risk of complications include:
- Smoking
This is an elective surgery. If you have any illnesses or you are in poor health for any reason, you should not undergo this procedure.
Silicone filled breast implants are not designed to last a lifetime. They typically need to be removed within 10 years. Your risk for complications increases the longer you have the implants.
What to Expect
Prior to Procedure
You may be asked to provide the doctor with a picture of a woman whose breasts you want yours to resemble. You may be asked to look through an album of breast sizes and shapes to help the doctor understand the outcome you desire.
Your doctor may do the following:
- Physical exam, including a careful breast exam
- Blood tests and urinalysis
- Electrocardiogram (ECG, EKG) —a test that records the heart’s activity by measuring electrical currents through the heart muscle
- Mammogram
- Chest x-ray
- Take “before” pictures
Talk to your doctor about your medicines. You may be asked to stop taking some medicines or herbal supplements up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as warfarin (Coumadin)
- Clopidogrel (Plavix)
- Gingko biloba or other herbal supplements
Leading up to your procedure:
- The night before, eat a light meal. Do not eat or drink anything after midnight.
- You may be asked to shower the morning of your procedure. You may be given special antibacterial soap to use.
- Arrange for a ride to and from the procedure.
- Arrange for help at home after returning from the hospital.
Anesthesia
Local anesthesia may be used, but general anesthesia is usually used. With general anesthesia, you will be asleep. With local anesthesia, the selected area will be numb.
Description of the Procedure
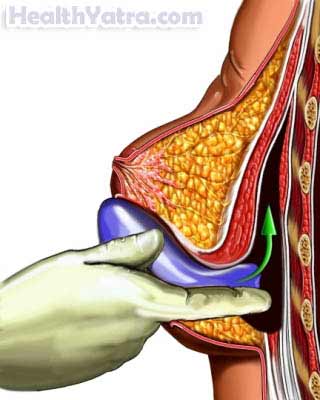
A cut in the skin will be made either underneath your breast, alongside the areola (pigmented area around the nipple), in your underarm, or in your belly button. An implant or prosthesis will be placed through the incision. The implant can contain silicone gel or can be filled with salt water (saline) after it is placed. It may be placed between the skin/breast tissue and the muscle, underneath the fascia (connective tissue of the muscle), or under the muscle itself. You may or may not have a drainage tube placed around the implant. The incision will be closed with stitches and bandaged. The same procedure may be repeated for the other breast.
How Long Will It Take?
About 1-2 hours
How Much Will It Hurt?
Anesthesia prevents pain during surgery. You may have some bruising and tenderness of the breasts for several weeks after surgery. Talk to your doctor about medicine to help manage the pain.
Average Hospital Stay
This procedure may be done in the hospital or surgery center. It may be possible to leave the hospital or surgery center on the same day of the procedure, or you may be asked to stay overnight in the hospital. Speak to your doctor about your options.
Post-procedure Care
- You will wear a special bra or bandage to put pressure on the breasts. This will help to support your breasts and decrease the chance of bleeding.
- You may wish to apply ice packs to your breasts to decrease swelling and pain. Wrap ice in a towel; do not apply ice directly to your skin.
- You may be given a prescription for pain medicine or advised to take acetaminophen or ibuprofen.
- Your doctor will advise you regarding return to exercise.
- Your doctor may advise you about massaging or moving your implants.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions.
Be sure that you follow-up with your doctor. For silicone gel implants, you will need routine MRI screenings to check for ruptures (tears or holes in the implant). The screenings are typically done three years after surgery and every two years after that.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Persistent elevated temperature
- Redness, swelling, increasing pain, excessive bleeding, or discharge at the incision site
- Fluid or blood collecting in either breast
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Pain that you cannot control with the medicines you have been given
- Implants grow hard, or you believe that they are leaking
- Cough, shortness of breath, or chest pain
- Pain and/or swelling in your feet, calves, or legs
- Joint pain, fatigue, stiffness, rash, or other new symptoms
In case of an emergency, call for medical help right away.
