Definition
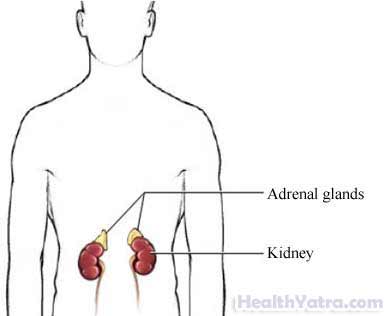
Adrenalectomy is the removal of one or both adrenal glands. There is one gland on top of each kidney. The adrenal glands make several hormones, including cortisol, aldosterone, and sex steroids.
Reasons for Procedure
Your adrenal gland may be removed if you have any of the following:
- Adrenal cancer
- Diseases of the adrenal gland, causing it to make too much of a hormone (eg, excess cortisol— Cushing’s syndrome, excess aldosterone—Conn’s syndrome, or excess adrenaline— pheochromocytoma)
- A large adrenal mass
- An adrenal mass that cannot be identified with a needle biopsy
Possible Complications
Complications from having an adrenalecomty may include:
- Insufficient cortisol production
- Decreases in blood pressure
- Bleeding
- Infections in the wound, urinary tract, or lungs
- Blood clots in the legs
- Injury to nearby organs or structures
- Adverse reaction to anesthesia
Factors that may increase the risk of complications include:
- Age: 60 or older
- Obesity
- Long-standing cortisol excess
- Smoking
- Poor nutrition
- Recent or chronic illness
- Heart or lung problems
- Alcoholism
- Use of certain medicines (eg, blood pressure pills, muscle relaxants, tranquilizers, sleeping pills, insulin, steroids, sedatives, or hypnotic agents)
- Use of street drugs (eg, LSD, hallucinogens, marijuana, or cocaine)
Be sure to discuss these risks with your doctor before the surgery.
What to Expect
Prior to Procedure
Your doctor will likely do some or all of the following:
- Physical exam
- Blood tests
- Urine tests
- Abdominal ultrasound —a test that uses sound waves to find specific places in the abdomen
- CT scan of the abdomen —a type of x-ray that uses a computer to make pictures of the kidneys and/or adrenal glands
- MRI scan —a test that uses magnetic waves to make pictures of the kidneys and/or adrenal glands
- CT scan of the head—to examine the pituitary gland (this gland controls the adrenal glands)
- Nuclear scan (MIBG or NP-59)—a test in which a small amount of radioactive material is injected and pictures are taken of the inside of the body to determine if the tumor is cancerous
- Give certain medicines to determine why the adrenal gland is not working correctly
Let your doctor know which medicines you are taking. You may be asked to stop taking or adjust the dose of certain medicines, such as:
- Aspirin or other anti-inflammatory drugs (may need to stop up to one week before)
- Blood-thinning medicines such as Warfarin (Coumadin)
- Clopidogrel (Plavix)
In the days leading up to your procedure:
- Arrange for a ride to and from the procedure.
- Arrange for help at home after the procedure.
- The night before, eat a light meal. Do not eat or drink anything after midnight.
- You may be given laxatives and/or an enema. These will clean out your intestines.
Your doctors may need to admit you to the hospital before your planned procedure if your blood pressure has not been well-controlled with medicines. This will allow more aggressive treatment to stabilize your blood pressure. It will also ensure that you have enough fluid in your body to prevent blood pressure problems after the surgery is done.
Anesthesia
General anesthesia will be used. You will be asleep.
Description of the Procedure
You will likely be given IV fluids, antibiotics, and steroid medicines.
Large masses are usually removed from the front of your abdomen. This is done so that the mass can be easily removed. The rest of your abdomen can also be examined.
An incision will be made just under your rib cage or in your abdomen. The adrenal gland will be carefully separated from the kidney. The gland will then be removed through the incision. The incision will be closed with either stitches or staples. It will be covered with a sterile dressing.
The doctor may choose to place a tiny, flexible tube into the area where the gland was removed. This tube will drain any fluids that may build up after surgery. It will be removed within one week after your operation.
Immediately After Procedure
The adrenal gland(s) will be sent to a lab to be examined. You will be sent to a recovery room. There, you will be monitored for any adverse reactions to the surgery or anesthesia.
How Long Will It Take?
1½ hours-3½ hours
How Much Will It Hurt?
Anesthesia prevents pain during surgery. Pain or soreness during recovery will be managed with pain medicine.
Average Hospital Stay
4-5 days
Postoperative Care
At the Hospital
- You will likely require pain medicines.
- You may be nauseated for a few hours after surgery. Your doctor may place a nasogastric tube through your nose and into your stomach to drain fluids and stomach acid. You will not be able to eat or drink until this is removed and you are no longer nauseated. In this case, you will continue to receive fluids through your vein. Once you begin eating, you may need to eat a lighter, blander diet than usual.
- You may be given special compression stockings to decrease the possibility of blood clots forming in your legs.
- Your body may be making substantially less natural steroid hormones. Your doctor may start you on steroid medicines immediately after surgery. The dose will then be tapered down.
At Home
Recovery time may be as long as 4-6 weeks. To help ensure a smooth recovery:
- You will need to be carefully monitored to see that your body is producing the right amount of steroid hormones or to verify that you are taking the correct dose of steroid medicine.
- You may be asked to weigh yourself daily and report any weight gain of two or more pounds over 24 hours. Such weight gain may indicate that you are retaining fluid. You may be asked to monitor your blood pressure regularly at home.
- Try to increase your physical activity according to your doctor’s instructions. This will help you avoid respiratory complications from the general anesthesia and improve the recovery of your digestive system.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions .
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision site
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Pain that you cannot control with the medicines you have been given
- Pain, burning, urgency, or frequency of urination; persistent bleeding in the urine
- Cough, shortness of breath, or chest pain
- Pain and/or swelling in your feet, calves, or legs
- Headaches
- Lightheadedness or dizziness
- Any new symptom
In case of an emergency, call for medical help right away.
