परिभाषा
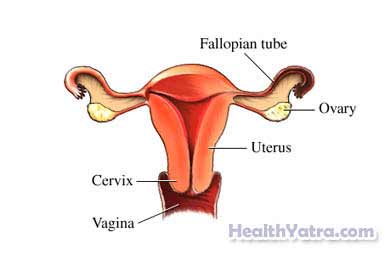
Dysplasia is abnormal growth or development of cells. Cervical dysplasia happens in the cells covering the surface of a woman’s cervix. If cervical dysplasia is not treated, it may lead to cervical cancer.
का कारण बनता है
Cervical dysplasia is caused by a sexually transmitted virus. The virus is called thehuman papillomavirus (HPV). This virus causes abnormal changes in the cells of the cervix. The most significant cervical change would be cancer.
There are different types of HPV. The risk of cervical disease may be high or low depending on the type of HPV.
जोखिम कारक
Factors that increase your risk of cervical dysplasia include:
- एकाधिक यौन साथी
- Early onset of sexual activity (before age 18)
- Early childbearing (before age 16)
- धूम्रपान
- Sexually transmitted diseases
- Genital herpes
- HIV
- Exposure to diethylstilbestrol (DES) in utero (in the womb)—an estrogen-like substance given to prevent miscarriages in high-risk pregnancies
लक्षण
There are often no apparent symptoms with cervical dysplasia. Cervical changes are found through screening tests.
निदान
Procedures to detect cervical dysplasia include the following:
पैप परीक्षण या पैप स्मियर जांच
Regular pap tests can help diagnose or monitor cervical dysplasia. Cells are collected from your cervix. They are sent to a lab for analysis. If abnormal cell growth is found, a colposcopy may be done.
HPV DNA Analysis
This will test for both the presence and type of HPV in cervical tissues. The presence of abnormal cells and high-risk HPV DNA increases the risk of significant disease. In this case, more evaluation and treatment will be needed.
Colposcopy and Biopsy
If further evaluation of the cervix is necessary, then a colposcopy will be performed. During this procedure, the cervix is lightly coated with a vinegar solution. The solution will highlight abnormal cells. A magnifying scope is then used to examine the cervix.
A biopsy will be done on any areas that show abnormal changes. A biopsy is the removal of tiny bits of tissue. A sample of the cells of the canal of the cervix will also be taken. This is done with a small brush. The biopsy and the sample of cells from the cervical canal will be sent to a lab for analysis. In the lab, abnormal cell growth will be classified as one of the following:
- Mild
- Moderate
- Severe (carinoma-in-situ)
- Invasive cervical cancer
उपचार
Treatment depends on the severity of dysplasia, location, and size of the area of abnormal cells. Some cervical changes do not need treatment. They may be followed by periodic Pap tests to monitor for any further changes. Some types of dysplasia may disappear on its own. If dysplasia does not resolve on its own, these treatments options are available:
Cone Biopsy
This biopsy is the removal of a tiny, cone-shaped piece of tissue. The sample is taken from the opening of the cervix and the cervical canal. The biopsy tissue will be analyzed. The results will show whether any of the abnormal cell growth is cancerous.
Loop Electrosurgical Excision Procedure (LEEP)
A small biopsy of the cervix is taken with a wire loop heated by electric current. The results will show whether any of the abnormal cells are precancerous or cancerous.
Note: Both cone biopsy and LEEP biopsy techniques remove all abnormal tissue. These procedures may be used for very early, noninvasive cancer treatment and diagnosis.
क्रायोसर्जरी
Cryosurgery freezes and destroys the dysplasia on the cervix. This method is not recommended for treating large areas of dysplasia.
Laser Treatment
Laser treatment uses a concentrated, high-energy beam of light to destroy abnormal cells. This method is more favorable than cryosurgery. There is less destruction of surrounding normal tissue. Although, healing is faster than with other methods and laser treatment is expensive. It is not always available.
Cancer Treatment
Cone biopsy and LEEP are usual cures for dysplasia. However, if the cone biopsy or LEEP biopsy shows invasive cancer, treatment methods may include:
- सर्जरी
- विकिरण चिकित्सा
- कीमोथेरपी
Your doctor will discuss these options with you.
Cervical dysplasia requires frequent follow up. Talk to you doctor about a Pap test schedule. A test may be scheduled every 3-6 months.
रोकथाम
जीवन शैली में परिवर्तन
To reduce the risk of cervical dysplasia, take these steps:
- Use safe sex methods to prevent HPV infection.
- If you smoke, quit.
- Get vaccinated against HPV infection. The HPV vaccine called Gardasil is approved for use in females aged 9-26 years old. The HPV vaccine called Cervarix is approved for females aged 10-25 years old.
अपने डॉक्टर से बात करें कि आपको पैप परीक्षण कब करवाना चाहिए। पेशेवर स्वास्थ्य संगठनों के अलग-अलग दिशानिर्देश हैं।
- If you are age 21-29 years, you should have the Pap test every two to three years.
- If you are age 30-65, you should have the Pap test along with the HPV test every three to five years.
- यदि आपकी आयु 65 वर्ष या उससे अधिक है, तो आप पैप और एचपीवी परीक्षण करवाना बंद कर सकते हैं यदि आपके परिणाम सामान्य हैं (जैसे, लगातार तीन सामान्य परिणाम और पिछले 10 वर्षों में कोई असामान्य परिणाम नहीं)।
- टिप्पणी: यदि आपके परिणाम असामान्य हैं तो आपको अधिक बार पैप परीक्षण कराने की आवश्यकता होगी। यदि आपको कुछ स्थितियां हैं, जैसे कमजोर प्रतिरक्षा प्रणाली या सर्वाइकल डिसप्लेसिया या सर्वाइकल कैंसर का इतिहास, तो आपको बार-बार परीक्षण की आवश्यकता हो सकती है। अपने लिए सही स्क्रीनिंग शेड्यूल के बारे में अपने डॉक्टर से बात करें।
