Definition
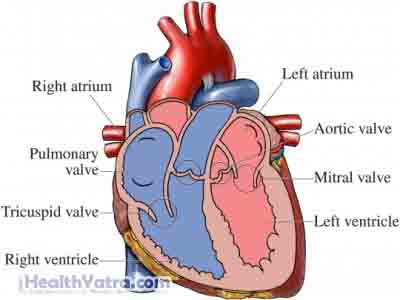
Ventricular tachycardia is an abnormally fast heart rate. The abnormal heart rate originates in one of the heart’s lower chambers (ventricles). It is diagnosed when there are three or more beats in succession originating from a ventricle. The heart beats at a rate greater than 100 beats per minute, but less than 200 beats per minute.
Ventricular tachycardia is considered sustained if it lasts more than 30 seconds. When this condition is sustained, the ventricles are not able to fill with enough blood for the heart to keep blood flowing properly through the body. This can result in lowered blood pressure, heart failure, and death.
Causes
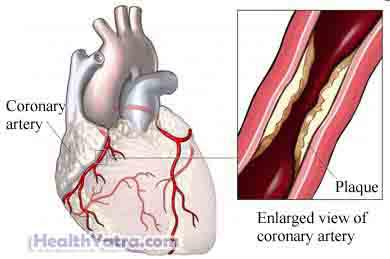
Damage to the ventricles can cause ventricular tachycardia. This damage to the heart muscle may be due to conditions like heart attack or cardiomyopathy.
Risk Factors
The following factors may increase your chance of ventricular tachycardia:
- Coronary artery disease
- History of heart attacks
- Heart abnormalities (eg, cardiomyopathy, mitral valve prolapse, valvular heart disease, ion channel disorders)
- Diagnosis of electrical instability
- Sarcoidosis
- Beginning treatment for hypothyroidism
- Use of certain medicines (eg, digitalis, antipsychotics, anti-arrhythmic drugs)
- Extreme physical or emotional overstimulation
- Low oxygen levels in the blood
- Very high levels of acid in bodily fluids (eg, due to kidney disease or diabetes)
- Stimulants (eg, caffeine, cocaine, alcohol)
Symptoms
Symptoms may include:
- A sensation of the heart beating very rapidly
- Feeling dizzy
- Feeling short of breath
- Fainting
- Chest discomfort
- Pale skin color
Diagnosis
This condition can be challenging to diagnose. Ventricular tachycardia often happens in emergency situations. It must be identified and treated very quickly.
To make the diagnosis, the doctor will order tests, such as:
- Electrocardiogram (ECG)
- Exercise stress test to test the heart’s performance
- Electrophysiology test to study the electrical signals of the heart
Treatment
In an emergency situation, CPR or a defibrillator may be required.
Other treatment options may include:
- Medicine, such as:
- Drugs to lower the heart rate (eg, lidocaine, procainamide, amiodarone)
- Beta-blockers to manage high blood pressure or heart rate
- Surgery, such as:
- Radiofrequency ablation
- Open heart surgery
If other approaches fail, an automatic defibrillator will be inserted into the heart to deliver shocks as needed to keep the heart rate steady.
Prevention
If you are at risk for ventricular tachycardia, your doctor may make these recommendations:
- Take beta-blockers to manage blood pressure.
- Take medicine to control heart rate.
- Get proper treatment for any underlying heart conditions that you may have.
- Avoid certain substances, such as caffeine, cocaine, and alcohol.
- Take steps to avoid heart disease, such as maintaining a healthy weight and exercising.
- If you smoke, quit.
