Definition
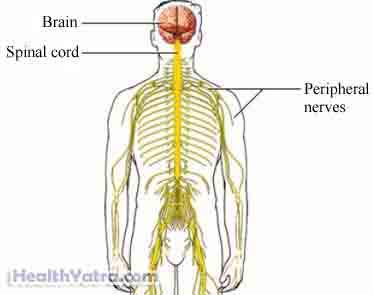
Rabies is an infection that affects the brain and spine. Rabies is almost always fatal unless treated before symptoms appear.
Causes
Rabies is caused by a virus. It is found in infected, warm-blooded animals. Animals that commonly carry the virus include:
- Bats
- Raccoons
- Skunks
- Foxes
- Coyotes
The virus is in the saliva, brain, or nerve tissue of infected animals. Humans most often contract rabies through a bite or scratch from an infected animal. The virus may also be passed if infected tissue comes into contact with skin in the eyes, nose, or mouth.
Risk Factors
The only risk factor is contact with an infected animal.
In most parts of the US any contact with a bat may be considered a rabies risk factor. Seek medical advice if you find a bat anywhere inside your home.
Symptoms
Symptoms often start within 3-7 weeks. In some cases, the virus can incubate up to one or more years. Death usually occurs within a week after symptoms appear.
Symptoms in humans may include:
- Pain, tingling, or itching at the site of the bite wound or other site of viral entry
- Stiff muscles
- Increased production of thick saliva
- Flu-like symptoms, such as headache, fever, fatigue, nausea
- Painful spasms and contractions of the throat when exposed to water
- Erratic, excited, or bizarre behavior
- Paralysis
Symptoms in animals may include:
- Erratic behavior, often overly aggressive or vicious
- Disorientation (for example, nocturnal animal such as a bat or fox appearing in daylight)
Diagnosis
If you think you have been exposed to rabies, see a doctor or contact a public health official immediately.
If the animal is available and appears well, it will be kept under observation to monitor its health. If no symptoms develop, you are not at risk for rabies. If the animal is sick or dead, it may be examined for the presence of the virus. In the meantime, you may be advised to begin treatment.
If the animal is unavailable, treatment may be given. The decision to give treatment maybe based on factors such as:
- Animal’s species
- Where the encounter took place
Treatment
If an animal has bitten you, immediately do the following:
- Wash the wound immediately with plenty of soap and water. It is the most important first step you can take in preventing rabies.
- Call your doctor or seek care in an emergency room.
If it is likely that you have been exposed to rabies, your doctor will recommend postexposure prophylaxis. This is treatment to prevent illness from developing. This treatment involves two injections:
Human Rabies Immune Globulin (HRIG)
This is given within 24 hours after exposure. It contains large amounts of antibodies to inactivate or destroy the rabies virus. In most cases, half of the dose is injected into the wound and surrounding tissue. The rest is given into a muscle. If you have previously received rabies vaccine, you may not need the HRIG shot.
Rabies Vaccines
Rabies vaccines make your immune system create antibodies against the virus. These antibodies will live in your body for many years. The vaccine is delivered in several shots over the next several weeks. The vaccine will be injected into your muscles.
There are several types of rabies vaccines available including the:
- Human diploid cell vaccine (HDCV)
- Purified chick embryo cell vaccine (PCECV)
Certain medication may interfere with your response to the rabies vaccine. Be sure to tell your doctor about all medicine or herbs that you take on a regular basis.
Prevention
To help prevent rabies:
- Vaccinate house pets.
- Avoid contact with wild animals.
- Do not touch any wild animal. Avoid it even if it appears to be dead.
- Seal basement, porch, and attic openings. This will prevent an animal from entering your home.
- Report any animal to your local animal control if it is acting strange or appears sick.
- If you often come in contact with potentially rabid animals, get the rabies vaccine before exposure. Booster doses are often needed.
