Definition
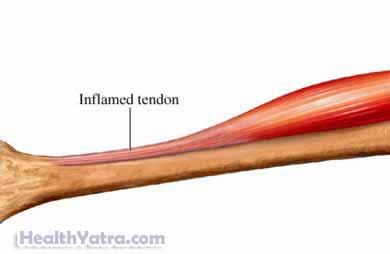
Tendinopathy is an injury to the tendon. It can cause pain, swelling, and limit movement. The injuries can include:
- Tendonitis—an inflammation of the tendon
- Tendinosis—tiny tears in the tendon with no significant inflammation
The posterior tibial tendon runs from the posterior tibial muscle to the inside of the ankle and the arch of the foot. The main job of this tendon is to support the arch of the foot. If the tendon is injured or weak the arch of the foot can collapse. This will make the foot pronate, or roll inward. These injuries can make it painful to walk.
Treatment depends on the severity of the tendinopathy.
Causes
Causes of posterior tibial tendinopathy include:
- Overuse of the tendon
- Poor blood supply to the tendon
- Biomechanics that cause degeneration of the tendon, such as over pronation of the foot
Risk Factors
Posterior tibial tendinopathy is more common in women and in people over the age of 40 years. Other factors that increase your chance of posterior tibial tendinopathy include:
- Flat feet
- Obesity
- Diabetes
- High blood pressure
- Previous surgery or trauma
- Local steroid injections
Symptoms
Symptoms may include:
- Pain and swelling near the arch of the foot and on the inside of the ankle
- Pain that increases when standing on the ball of the foot or if the foot is flexed
- Pain that increases with activity
- Tiredness in the foot after little activity
- Pain that becomes more disabling
- Later in the course of the tendinopathy, a flattening of the arch of the foot and pronation
- An inability to push off well when running
Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done. Pain in the foot and ankle can be due to many causes. Posterior tibialis tendinopathy can be difficult to diagnose.
The doctor will try to feel the tendon through your skin. He will note how the foot moves and handles resistance to moving the foot inwards. The doctor will look at the foot from behind and from the side and see how flat the arch is. You may be asked to try to stand on the ball of your foot. If you cannot do this you are likely to have a problem with your posterior tibial tendon.
Your doctor may recommend image tests to see the the structure of the foot and ankle. Tests may include:
- X-rays
- MRI
- Ultrasound
Treatment
Talk to your doctor about the best treatment plan for you. Options include:
Home Care
To reduce pain and swelling:
- Avoid activity that causes pain. Reduce shock or vibrations to the foot and ankle.
- Apply an ice pack for 15-20 minutes at a time, several times a day. Place a towel between the ice pack and your skin.
- Wrap your injured foot in elastic bandaging. Don’t wrap the bandage too tight. It may cut off circulation.
- Elevate your foot above your heart.
To help support the foot and promote healing, you may need:
- A strap or tape for your foot
- A brace or cast
- Custom-made orthotics
Medication
To help manage pain, your doctor may recommend:
- Over-the-counter pain relievers, such as acetaminophen or non-steroidal anti-inflammatory medication (NSAIDs)
- Topical pain medications that are applied to the skin
- Prescription pain relievers
Physical Therapy
Physical therapy will help:
- Stretch and condition the the posterior tibial muscles
- Maintain muscle strength, flexibility, and endurance
- Improve balance and range of motion
Surgery
In rare cases, surgery may be required to repair the tendon.
Prevention
To reduce your chances of posterior tibialis tendinopathy, take these steps:
- Avoiding activities and sports that repeatedly stress the foot and ankle.
- Maintain proper muscle strength.
- Gradually increasing the frequency and intensity of exercise.
- Wear good, supportive shoes that provide arch support.
- Use proper technique for sports and dance activities.
