Definition
Polyarteritis nodosa is an autoimmune disease. Your immune system is your body’s defense system. It fights diseases and infections. An autoimmune disease is a condition in which your body’s immune system mistakenly attacks your own body. With polyarteritis nodosa, medium-sized arteries and, less commonly, small arteries (blood vessels that carry blood from the heart to the rest of the body) become inflamed and damaged. The inflammation of the arteries affects many different organs, including the:
- Skin
- Central nervous system (part of the nervous system that includes the brain and spinal cord)
- Peripheral nerves (nerves of the feet, hands, legs, arms, and face)
- Gastrointestinal tract (part of the digestive system that includes the mouth, esophagus, stomach, and intestines)
- Kidneys
- Heart
- Joints
- Ear, nose, and throat
Although polyarteritis nodosa is a rare disease, it is a potentially serious condition that requires care from your doctor. The sooner it is treated, the better the outcome. If you suspect you have this condition, contact your doctor right away.
Causes
The cause of polyarteritis nodosa is unknown. In relatively rare cases, however, it occurs with hepatitis B virus infection or hairy cell leukemia.
Risk Factors
A risk factor is something that increases your chance of getting a disease or condition. The following factors increase your chance of developing polyarteritis nodosa:
- Age: 40 to 60 year olds—Although it can occur at any age, it occurs most middle-aged adults. The incidence raises with age.
- More common in males
- Hepatitis B or hepatitis C infection
- Hairy cell leukemia
- Intravenous drug use
Symptoms
Polyarteritis nodosa is a multisystem disease. This means that it affects many parts of your body at the same time. It has a tendency to affect organs such as the skin, kidney, nerves, and gastrointestinal tract (part of the digestive system that includes the mouth, esophagus, stomach, and intestines).
If you experience any of these symptoms, do not assume it is due to polyarteritis nodosa. These symptoms may be caused by other, less serious health conditions. If you experience any one of these, see your doctor.
Often with polyarteritis nodosa you will experience fatigue, weight loss, loss of appetite, and fever. Symptoms affecting particular organs include:
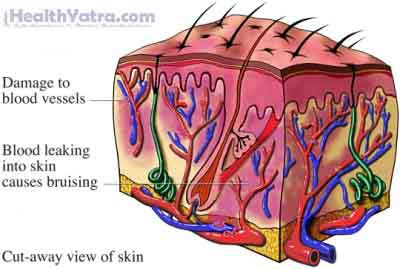
- Skin–polyarteritis nodosa often affects the skin first, especially on the legs, causing:
- Rashes
- Ulcers (open sores on the skin)
- Nodules (small bumps under the skin)
- Bruises
- Gangrene (blood supply to the tissues is stopped, causing the skin to die)
- Nervous system
- Tingling, burning, pain, or numbness in your feet, hands, legs, arms, and face
- Seizures
- Stroke (rare)
- Decreased alertness
- Inability to think clearly
- Kidneys
- Protein in the urine
- Hypertension (high blood pressure)
- Gastrointestinal
- Pain in the abdomen
- Gastrointestinal bleeding
- Bowel infarction (not enough oxygen-rich blood to the bowels causing tissue damage)
- Nausea, vomiting
- Bloody and non-bloody diarrhea
- Heart
- Heart attacks (heart does not get enough blood flow leading to the death of the heart muscle)
- Congestive heart failure (inability of the heart to pump out all the blood)
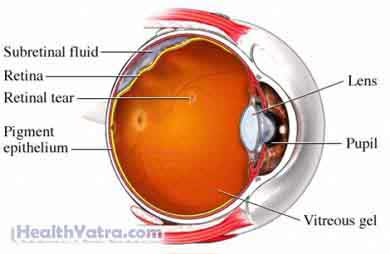
- Eyes
- Detachment of retina
- Scleritis—inflammation in the sclera (white part of the eye)
- Genitals
- Testicular infarction (not enough oxygen-rich blood to the testicles causing tissue damage)
Diagnosis
There is no single test to diagnose polyarteritis nodosa. Your doctor will ask about your symptoms and medical history, and perform a physical exam.
Tests may include the following:
- Blood tests
- Elevated ESRs ( erythrocyte sedimentation rate ) and CRP ( C-reactive protein )—to measure the degree of inflammation and to monitor inflammatory disease
- CBC ( complete blood count )—to look for elevated white blood count
- Kidney function tests
- Liver function tests
- Hepatitis blood tests
- Immunoglobulins: to look for elevated levels of this blood protein that functions in immunity
- Urine test—to check for protein in the urine
- Skin biopsy —surgical removal of some skin for further examination
- Biopsy of muscles, nerves, kidney, or bowel—surgical removal of a sample of muscle or nerve to see if there is evidence of arterial inflammation in those tissues
- Nerve conduction study—to evaluate for muscle or nerve damage
- Your doctor will place small electrodes on your skin over the muscles being tested; electrical signals produced by your nerves and muscles are recorded, and the information is interpreted by a specially-trained physician.
- Arteriogram—dye is injected in arteries, and x-rays are taken that can reveal inflammation within the vascular system
Treatment
Early diagnosis and treatment of polyarteritis nodosa may improve the outcome. Treatment should be vigorous, with the goal being to reduce the inflammation of the arteries and put the condition into remission (period during which symptoms of a disease disappear).
Without treatment, the condition may be fatal. Complications from polyarteritis nodosa include stroke, kidney failure, heart attack, and permanent tissue damage of the intestines.
Talk with your doctor about the best treatment plan for you. Treatment options include the following:
- Corticosteroids—High doses of these steroids, by injection or by mouth, can reduce inflammation of the arteries.
- Immunosuppressive drugs—Suppressing the immune system helps decrease inflammation of the arteries by countering the body’s autoimmune reaction.
- Antiviral drugs—When hepatitis B or C is present, antiviral medications are helpful in addition to immunosuppressive drugs.
Prevention
There is nothing you can do to prevent polyarteritis nodosa.
