Definition
Paroxysmal supraventricular tachycardia (PSVT) is an abnormally fast heart beat, that begins and ends suddenly. While the normal resting heart rate is approximately 60-100 beats per minute, a PVST attack may cause a heart rate as fast as 160-280 beats per minute. People with PVST have attacks of tachycardia that can last anywhere from a few minutes to several hours. The abnormal heart rate originates in heart tissue other than the ventricles or lower chambers of the heart
Although PVST is not usually life-threatening, it can cause symptoms including palpitations or feeling of heart racing, light-headedness, chest discomfort, and rarely loss of consciousness. Frequent and prolonged episodes, if not treated, can cause weakening of the heart muscle. This can result in an inability of the heart to pump effectively. This may limit a person’s physical activity. If you suspect you have this condition, contact your doctor to discuss diagnosis and treatment options.
Causes
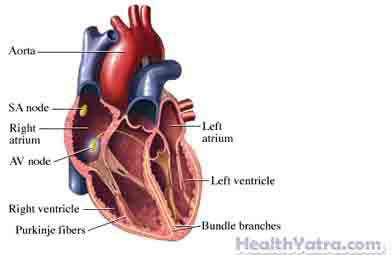
In a normal heart, electrical impulses from the heart’s natural pacemaker, the sinoatrial or SA-node, prompt the heart to pump blood throughout the body. PVST is the result of a “short circuit” in the electrical system of the heart. Normally there is only one electrical pathway between the upper chambers of the heart (the atria) and the bottom chambers (the ventricles). This connection is called the atrioventricular or AV-node. In some cases, the AV-node has two pathways which can conduct impulses, a slow pathway and a fast pathway. This creates a situation in which a feedback loop can occur called re-entry. Other patients have an abnormal, additional connection between the atria and ventricles called an accessory pathway leading to PSVT. Still others have an irritable group of cells in the atria that drives the tachycardia.
Risk Factors
There are several factors that may increase your chance of having an attack or developing symptoms. In general, PVST:
- Affects women more often than men
- Most commonly develops in a person’s 20s or 30s, but can occur at any age
- Occurs more often in people who are anxious, under stress, or physically fatigued
- Hyperactive thyroid gland
- Excess caffeine or alcohol use
- Respiratory illnesses
- Low potassium and magnesium levels
- Valvular heart disease
Symptoms
If you experience any of these symptoms, do not assume it is due to PVST. These symptoms may be caused by other, less serious health conditions. If you experience any one of them, see your physician.
- Rapid heartbeat or palpitations
- Weakness, dizziness, or feeling faint
- Shortness of breath and anxiety
- Chest discomfort
- Rarely, loss of consciousness
Diagnosis
A diagnosis of PVST usually begins when a person notices uncomfortable attacks of rapid heart beating. Your doctor will ask about your symptoms and medical history, and perform a physical exam. The attacks may be too brief for the doctor to observe, so tests may be ordered to find the cause of the attacks. Tests may include the following:
- Electrocardiogram (EEG) —measures the electrical activity of the heart
- Implantable loop recorder (ILR) is a small device that is surgically implanted under the skin of the chest and can be left in place for up to a year, or longer in some cases, in order to diagnose abnormal heart rhythms.
- Electrophysiologic study (EPS) is an invasive heart study where electrical wires are placed in the heart through a small puncture in the veins in groin. These wires map the electrical conduction system of the heart to locate the source of the abnormality.
- Echocardiogram or ultrasound exam of the heart to exclude structural heart disease
- Blood tests to look for abnormalities in electrolytes and thyroid function
Treatment
Treatment for PVST involves stopping the electrical impulses causing the attacks. This can be attempted manually by your doctor using several techniques, including a guided breathing exercise called the Valsalva maneuver or carotid sinus massage. With the latter technique, the doctor applies pressure to the carotid artery in the neck for a few seconds, to reset the electrical signals, and return the heart rhythm to normal. The doctor may teach you to do these procedures to do yourself to terminate the episodes.
If manual methods fail, additional options include:
Pharmacological Methods
For people who have numerous attacks, there are drugs available that can slow the conduction of electrical signals. These include:
- Calcium channel blockers such as verapamil (Calan) or diltiazem (Cardizem)
- Digoxin
- Beta-blockers such as atenolol or metoprolol (Lopressor)
- Antiarrhythmic medications
Surgery
A surgical procedure, known as ablation, may be necessary if attacks are frequent or the patient does not want to take medications. In this therapy, the abnormal portion of cardiac tissue causing the arrhythmia is identified and destroyed. This procedure is done in conjunction with an electrophysiology study.
Prevention
- Limit alcohol, smoking, and caffeine
- Avoid stressful situations
- Avoid excessive fatigue and lack of sleep
