Definition
Fecal incontinence is the loss of control over the bowels. Some people may have uncontrolled release of just gas and liquid stool. Others have no control over the release of solid waste. Many people with this condition also have trouble controlling the release of urine.
This condition can lead to issues, such as depression or isolation. If you think you have this condition, contact your doctor right away.
Causes
Women are more likely to suffer from this condition than men are. Many cases are a result of an injury to the pelvic floor. The pelvic floor is a group of muscles that support pelvic organs. Injury can happen through pregnancy or delivery. Other causes include:
- Constipation
- Rectal prolapse
- Congenital abnormality (condition present from birth)
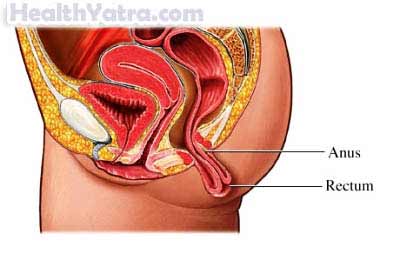
- Trauma or injury to anal sphincter or its nerves (the healthy sphincter opens and closes to control the release of fecal material)
- Diarrhea
- Scarring of the rectum from irritable bowel syndrome, radiation therapy, or surgery
- Anal abscess or perirectal abscess
Risk Factors
Risk factors include:
- Gender: female
- History of episiotomy
- Older age
- Diseases of the nervous system (eg, stroke)
- Damage to the spinal cord (eg, cauda equina syndrome)
- Other risk factors thought to contribute to fecal incontinence include:
- Diabetes
- Depression
- Lack of physical activity
- Being overweight
Symptoms
The main symptom is the inability to control bowel movements, which leads to stool leakage.
When Should I Call My Doctor?
Call your doctor if you have fecal incontinence. Your doctor can help find the underlying cause.
Diagnosis
Your doctor will ask about your symptoms and medical history. A physical exam will be done. Your doctor may send you to a specialist, such as:
- Gastroenterologist
- Colorectal surgeon
- Proctologist
Tests may include the following:
- Anorectal manometry—test that uses a catheter to check pressure in the anal canal while resting and squeezing
- Pudendal nerve terminal motor latency (PNTML) testing—test that uses an electrode in the anal canal to evaluate how well the nerves are working
- Endoanal ultrasound—test that uses sound waves to make a picture; used to detect any injury to anal sphincter muscles
- Proctosigmoidoscopy—test that uses a thin, lighted tube inside the rectum; used to examine the rectum and lower colon for injury or disease
- Defecography—test that uses x-rays and dye to look at the bowel and how it functions
Treatment
Talk with your doctor about the best plan for you. Options include:
Diet
Your doctor may suggest changes to your diet. You may be referred to a nutritionist for diet ideas. Examples of dietary changes include:
- Eating smaller meals more frequently
- Avoiding foods that may trigger diarrhea (Spicy food or foods with caffeine are common culprits.)
- Eating more fiber and drinking more fluids (if incontinence is due to constipation)
Devices
Absorbent diapers are often used with fecal incontinence. Another option is an anal plug. These plugs, which are available in a variety sizes and shapes, may be helpful for some people to control symptoms.
Bowel Training
Your doctor may suggest using biofeedback. This method can retrain your body’s responses.
A bowel movement schedule can also train your bowels. For example, you can pick four times throughout the day to try to go to the bathroom.
Exercise
Learn how to do Kegel exercises. These exercises help strengthen the pelvic floor muscles.
Surgery
Surgical procedures may be used to treat this condition when other treatments have failed. Examples include:
- An overlapping sphincteroplasty to rebuild the anal sphincter
- Injecting bulking agents, radiofrequency therapy, and/or nerve stimulation
- Inserting an artificial bowel sphincter (which you can open and close as needed)
- Colostomy (done in severe cases)—disconnects the colon and brings the end through an opening in the abdomen
Prevention
To help reduce your chance of getting fecal incontinence, take the following steps:
- Prevent constipation by eating a high-fiber diet and drinking plenty of fluids.
- Pay attention to your diet and avoid foods that trigger diarrhea.
- Try to maintain a regular bowel movement schedule.
- Talk to your doctor if you are having trouble with diarrhea or constipation.
